Abstract
INTRODUCTION: Chronic inflammation and immune stimulation have been linked to the development of myelodysplastic syndrome (MDS) and acute myeloid leukemia (AML). Abnormal production of adipokines in obesity is known to cause increased oxidative stress and low-grade chronic systemic inflammation. Previous retrospective studies have reported that obesity was associated with increased risk of developing MDS and AML. It has also been suggested that obesity may be an adverse prognostic factor in MDS, resulting in decreased overall survival (OS) and increased risk of conversion to AML in certain subsets of MDS patients, particularly those with lower-risk disease. We sought to further define clinical characteristics associated with obesity in lower-risk MDS.
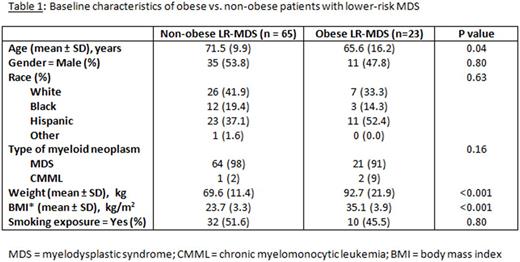
METHODS: We used our institution's data mining software to identify patients with biopsy-proven MDS or CMML diagnosed between 2001 and 2016. 88 patients with lower-risk disease (Very Low, Low or Intermediate risk by IPSS-R score) with a body mass index (BMI) documented at the time of diagnosis were selected for this retrospective study. 23 patients had a BMI ≥ 30 (Obese LR-MDS) and 65 patients had a BMI <30 (Non-obese LR-MDS). Patient demographics (Table 1), hematologic parameters, cytogenetics, rate of conversion to AML and ultimate need for treatment with hypomethylating agents were compared between both groups. Survival analysis was conducted using the Kaplan-Meier (KM) method.
RESULTS: Mean BMI was 35.1 kg/m2 in Obese LR-MDS and 23.7 kg/m2 in Non-Obese LR-MDS. Obese LR-MDS patients presented at a significantly younger age (mean age 66 vs. 72, p=0.04). Baseline hemoglobin was significantly lower in the Obese LR-MDS group (mean 8.4 vs. 9.3 g/dL, p=0.03) and so was baseline platelet count (mean 91 vs. 149 x 103/µL, p=0.03). Differences in OS between the two groups were non-significant. Rate of conversion to AML was higher in the Obese LR-MDS group but the difference was not statistically significant (17.4% vs. 6.2%, p=0.23). A higher proportion of patients in the Obese LR-MDS group ultimately required treatment with hypomethylating agents but difference was not statistically significant (39.1% vs. 21.5%, p=0.17). No cytogenetic anomalies were seen at a higher rate in the Obese LR-MDS group.
CONCLUSION: Obese patients with lower-risk MDS in our analysis presented at a significantly younger age and had more severe anemia and thrombocytopenia at the time of diagnosis than non-obese patients. The significant differences in hemoglobin and platelet count are strongly suggestive of dysfunctional hematopoiesis in obese lower-risk MDS patients. We were not able to corroborate the previously reported findings of decreased OS or increased risk of conversion to AML in this population. We hope to refine our data further with mutational analysis to delineate whether certain mutations have a strong association with obesity and lower-risk MDS.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.